
A tiny microbe has turned the world upside down. As of April 22, the Johns Hopkins University Coronavirus Resource Center (JHU-CRC) reports that 210 countries or territories have confirmed the presence of COVID-19 cases. The JHU-CRC confirms 2,636,414 cases and 184,204 deaths worldwide.
How did we get here? On December 31, 2019, reports began to circulate of a large number of cases of pneumonia-like illnesses among people associated with a seafood market in Central China. On January 7, 2020, Chinese health officials confirmed these reports, when they announced the discovery of a new strain of a coronavirus. This new virus was named n-2019CoV, or COVID-19.
On January 11, Chinese media reported the death of the first victim of COVID-19 in China. This report came days before the Chinese New Year, which is the biggest holiday of the year. During the week-long celebration, people usually travel hundreds of miles to be with family and friends. By January 20, Chinese media reported more than 700 cases and at least a dozen deaths in Wuhan.

On January 23, the Chinese government shut down the whole city of Wuhan and ordered its population of 11 million people to shelter in place. This action was an attempt to wall the virus off from the rest of the world. But the spread had already begun.
By January 20, Japan, South Korea, and Thailand reported cases. On January 21, the United States reported its first case. It was a man in Washington state, who had recently returned from a trip to Wuhan.
In February, Wuhan was the epicenter of a worldwide pandemic. In March, the epicenter switched to Europe. Italy, Spain, and France reported thousands of cases and hundreds of deaths. Today, the United States is the epicenter of the pandemic.

As of April 20, there are 817,187 confirmed cases of COVID-19. A total of 45,229 deaths in the United States have been attributed to this coronavirus. Since early April, all 50 states in the United States have put some type of lock-down or shelter-in-place restrictions in place. Social distancing guidelines are also in effect.
Large gatherings are banned. This includes schools, church services, concerts, political rallies, and sporting events. Non-essential businesses are closed. Restaurants and bars can only offer take-out or delivery services. Individuals are ordered to only leave their homes for groceries and other essential goods, medicines, or medical appointments. If you do venture out, masks that covered your mouth and nose are required.

American primary, secondary, and higher education institutions were all forced to turn on a dime. Schools were shuttered. College students on spring break were ordered not to return to campus. Those students on campus were told to leave and return home. All face-to-face classes were suspended. Teachers and students were forced to finish the remainder of the spring terms remotely. As the lockdown continued, dissatisfaction among the ranks of faculty, students, and parents grew.

Commencements and other celebrations which, for as long as the current higher education crowds can remember, have always closed out the school year were canceled. Most traditional summer schools have been abandoned. Events for new students have been indefinitely put on hold. Even now in mid-April, the fall semester is still a big question mark. These pivots were all huge changes. They could not be as easily accomplished as flipping a light switch.
Are more changes in American higher education inevitable? Will schools be allowed to hold face-to-face classes in the fall? Will students pay F2F rates for online classes? Will students reenroll in their schools in the fall or will they transfer to another college or drop out of school completely? Will new students enroll at the rates colleges have come to expect? Will faculty accept the changes to their routines? How will state and federal governments and the general public support the changes in higher education? What will the new norm for American higher education look like?
Hospitals and medical professionals were forced into war-zone like activity. Everyone’s attention was turned to the diagnosis and treatment of COVID-19. Entire hospitals were devoted to just COVID-19 patients. Large facilities like sports and conference arenas, hotels, and cathedrals were converted into temporary hospitals. Emergency hospitals were constructed in days, instead of years, to meet the surging needs.
We don’t know how many people have been hospitalized because of the COVID-19 pandemic. In March, Vice President, Mike Pense, sent a letter to the administrators of the nation’s 6,000 hospitals asking them to inform the Center for Disease Control and Prevention(CDC) each day of the number of patients that they were currently treating for the virus.
It is not clear how many hospitals have complied with VP Pense’s request. The CDC has not released any reports on these data. When asked, CDC officials only say that it is under review and will be released shortly. Various states and cities have released hospitalization reports. However, these jurisdictions have used their own definitions and the data may not be consistent.

It doesn’t seem possible that almost a decade ago I wrote two posts that compared the American higher education enterprise to the four disparate industries. In the first post, I asked the provocative question What can American higher education learn from the watch industry, the chocolate industry, and toilet paper manufacturers?

In the second post, Comparison of American Higher Education with the Automotive Industry For many educational purists, I did the unthinkable of comparing American higher education to the struggling automotive industry.
In those posts, I suggested that higher education could face great disruptions similar to the disruptions that those other industries have endured. In this post, I will be brave and take my comparison one step further.

The coronavirus has shined a spotlight on both the health care profession and the higher education enterprise. With both industries under siege from this common enemy, I see a number of striking similarities.
The first similarity is that both have a strict dichotomy between the professionals and the clients, those served by the professionals. It is a great divide between the experts and the untrained. In both fields, the experts provide the untrained with specific services. In medicine, untrained patients are treated by expert medical professionals. In education, the untrained students are taught by the expert faculty.

The second similarity relates to the hierarchical structure among the professionals in both fields. In higher education, faculty members strive to climb the professorial ladder to the top position of a tenured, full professor. Beneath those individuals who made it to the top rung are the associate and assistant professors, the instructors, the adjunct and contingent faculty members, and the lowly graduate assistants. In medicine, the specialists are at the top of the ladder. Under them stand the general practitioners or primary care physicians, the physician assistants, and nurse practitioners. Near the bottom are the registered nurses. On the bottom rung are the practical nurses and medical technicians.

The higher rungs translate into more prestige. The higher rungs on the disciplinary ladders also carry with them increased monetary rewards. In addition, the higher rungs mean increased responsibility. Unfortunately, more often than not, the individuals on the lower rungs get loaded with more of the direct contact work with the patients and students.

The third similarity shared by both fields is the primary, preferred mode of the delivery of services. For many centuries, this primary mode of delivery of service has been face-to-face. I almost said “up-close and personal.” This is definitely true in medicine. However, higher education started to move away from tutorials and small classes in the lower-level courses to large classes in the twentieth century. Only a few elitist, high-priced institutions held on to the small classes and seminar format for all courses. Even in graduate schools, one-on-one work between a student and a professor is reserved for theses or dissertations.
Since the middle of the 20th Century, many social commentators have addressed the fourth similarity I see between healthcare and higher education. The current pandemic brings the same critical deficiency in both fields to the forefront of the public interest.

The problem is that there is a huge gap in the quality of service within higher education and healthcare available to individuals across racial and ethnic groups, as well as social and economic strata. Certain groups and individuals are privileged. Individuals with economic means have available the best healthcare and education that money can buy. They have access to the best colleges, doctors, and hospitals.

Other groups and individuals are greatly disadvantaged. As a group, minorities and poor individuals tend to “get the left-overs.” There are exceptions, but a much larger percentage of those adversely affected by the coronavirus are the minorities and the poor.
As an example, in a small city near my home, the coronavirus disproportionately affected the minority communities. The total population of the city is 40% White (non-Hispanic), 25% African-American, 30% Hispanic/Latino, and 5% Other. However, in the early coronavirus counts, 70% of confirmed cases and deaths were in the Hispanic/Latino community, and 20% in the African-American community.
The fourth similarity reminded me of my high school Latin. If you studied Latin, you will remember “Gallia est omnis divisa in partes tres”. [All Gaul is divided into three parts.] This is the opening line of The Gallic Wars by Julius Caesar. Everyone who studied high school Latin in the mid-twentieth century was required to translate Caesar’s classic journal. What has this to do with medicine and higher education?
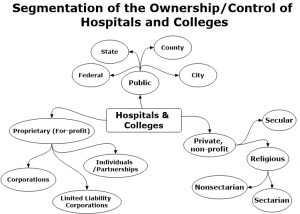
The ownership or control of all medical and higher education institutions falls into three segments. These three groups are:
- Public: These institutions are controlled or owned by a government entity such as the country, a city, county, state, or an agency of one of the above. The two primary sources of funding are government support or fees for service.
- Private, non-profit: These institutions are owned by a private, non-profit foundation or corporation. They are controlled by a self-perpetuating Board of Trustees. The two primary sources of funding are fees for services or the Board through charitable fundraising efforts.
- Proprietary: Another name for these institutions is Private, for-profit. They are owned by individuals or for-profit corporations. They are controlled by the owners or a Board of Trustees elected or appointed by the owners. The primary source of funding is through fees for services. The expectation is that these institutions will make a profit for their owners.

Since higher education and healthcare are both divided into three segments of control and ownership, they face the same set of challenges and advantages. For decades, the two fields have claimed that the challenges far outnumbered the advantages. Since I am running out of time and space in this post, I will leave the discussion of the challenges and advantages to another post.
At this time, I plan to publish that post on Friday, May 1. On Monday, April 27, I will be publishing a special announcement. I am changing the format of By’s Musings again.
During the week of April 27, I will be previewing a monthly newsletter, which will highlight what I am reading and listening to in the field of higher education. It will point readers to upcoming webinars (mostly free) and significant higher education articles that have appeared in the previous month. It will discuss the trends and challenges facing higher education. Special features of future issues will include book reviews, interviews of higher education leaders, and invited articles from experts in the fields of higher education, leadership, and organizational development.
After this first issue in my blog, I will be asking readers to subscribe to the newsletter. It will begin as a free offer. However, in the interest of full disclosure, I will be looking for ways to monetize this effort. I do promise that I will keep the subscription cost-free as long as I can.

With the addition of this newsletter, I will reserve By’s Musings for my reflections on life in general, as well as my faith and health journeys.
In the meantime, stay safe and healthy. Remain vigilant. Eat healthily. Maintain the practice of your spiritual disciplines. Practice social distancing, but remain in close social contact with family, friends, and colleagues.
Leave a Reply